Your Pharmacy’s Guide to Key Medicare Part D Changes in 2019 – Part 2

Welcome back to our discussion of 2019’s key changes in Medicare Part D, and how those changes are poised to impact the operations and relationships of independent pharmacies.
In Part 1, we discussed the addition of new policies aimed at curtailing the opioid addiction epidemic in America. We also discussed changes to patient coverage that affect the coverage gap, or “donut hole,” and the resulting potential impact on a patient’s finances.
Today, we’ll look at a few more changes, including:
- “Any willing pharmacy” term clarification aiming to increase participation from non-traditional pharmacies
- Formulary flexibility that allows plans to substitute or remove brand-name drugs
- New Medicare cards issued this year that patients must use by 2020
Let’s dive in.
Increased Participation in Part D Plans
The “any willing pharmacy” provision (AWP) already exists for all Part D plans, stating that any pharmacy meeting the standard terms of contracts should be included in preferred and/or standard pharmacy networks.
In this version, “standard terms and conditions” varied based on different pharmacy types and geographic areas – as long as the same terms were offered to “similarly situated” pharmacies.
However, some pharmacy benefit managers (PBMs) still excluded certain pharmacies they deemed non-traditional, such as community pharmacies offering home delivery via mail, pharmacies selling durable medical equipment, or specialty pharmacies treating one or more disease states requiring complicated therapy regimens. These PBMs claimed that these pharmacies weren’t “similarly situated.”
The new language clarifies that any pharmacy can comply with the standard terms and conditions for a specific pharmacy type, even if it doesn’t exclusively operate as that pharmacy type.
Takeaway for pharmacies: You’ll find more options to participate in Part D plans, even if you have non-traditional operations. And, as an AlliantRx member, we can help guide you toward more options.
Formulary Flexibility
 Under current formulary rules, Part D plan sponsors are permitted to add generics, but they’re not permitted to remove brand-name versions unless they:
Under current formulary rules, Part D plan sponsors are permitted to add generics, but they’re not permitted to remove brand-name versions unless they:
- Obtain approval from CMS
- Give 60 days’ written notice of the upcoming cost increase
- Guarantee that beneficiaries will receive access to a transitional fill of that brand-name drug
However, the new Medicare Part D changes allow plan sponsors to change their formularies immediately and without warning — they can move brand-name drugs to lower tiers or replace them completely with newly approved generics that have been labeled therapeutically equivalent.
This means that patients may feel blindsided when they go to pick up their medications, only to realize that they must pay more or switch to a generically equivalent drug. This will be especially difficult for patients whose prescriptions are labeled “dispense as written,” which may require pharmacists to dispense a particular drug that’s no longer available.
Takeaway for pharmacies: You may need to provide extra support to patients who haven’t been previously warned about price increases or switches to generics.
New Medicare Cards for Patients
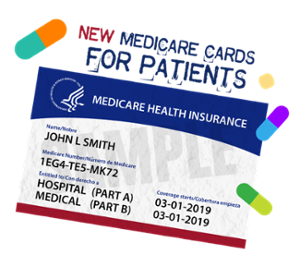 Beginning January 1, 2020, Medicare beneficiaries will be required to use a special new card with a Medicare identification number. Mailing for these cards began in April 2018 and will continue through April 2019.
Beginning January 1, 2020, Medicare beneficiaries will be required to use a special new card with a Medicare identification number. Mailing for these cards began in April 2018 and will continue through April 2019.
If you’d like to know when your state’s beneficiaries received or will receive their cards, visit the CMS website here.
Takeaway for pharmacies: You’ll need to ensure that your pharmacy system’s information is updated. Remember to keep this top-of-mind for your staff and patients.
Closing Thoughts
As we move through 2019, it’s important for pharmacies to stay on top of Medicare Part D changes that have recently gone into effect. By staying educated and prepared, pharmacies have the ability to mitigate issues while providing support to the patients who may need it most.
If you’re not yet an AlliantRx member, 2019 is your year to join us. If you are already a member, be sure to leverage your benefits to maximize yours and your patients’ success with Medicare Part D’s 2019 benefit changes.
Has your pharmacy already experienced any impacts from changes that just went into effect? Do you have any stories, advice, or strategies to share with other specialty pharmacies?
We’d love to hear about it—and even possibly share your experiences in our future blog posts, e-books, and white papers. If you’d like to share your experience, contact Jessica Gardner.
